Personalized thermal therapy represents an advanced treatment modality for managing chronic and acute pain conditions. It involves precise temperature application tailored to individual patient needs, enhancing blood circulation, reducing inflammation, and aiding cell repair. This therapy is versatile, using methods ranging from traditional ice packs to sophisticated equipment like focused ultrasound devices for targeted deep-heat treatment. The personalization of intensity and duration, informed by patient feedback, aims to improve pain relief outcomes while minimizing side effects, thus providing a safer healing environment. Ongoing evaluations and therapy adjustments are crucial for responsive treatment throughout the recovery process, ensuring that thermal therapy remains effective and comfortable for the specific pathology involved. This personalized approach underscores the importance of thermal therapy in enhancing pain management outcomes, with a focus on creating a therapy regimen that is both tailored to individual needs and conducive to healing and comfort.
Exploring the transformative potential of personalized thermal therapy for pain relief, this article delves into the nuanced approaches that tailor temperature variations to individual needs. We will navigate through the spectrum of thermal therapy techniques, illuminating their application in effective pain management strategies. From understanding the principles behind these treatments to crafting a bespoke regimen, readers will gain insights into the practical application of thermal therapy for optimal health benefits. Join us as we dissect the mechanisms and methods that make thermal therapy a compelling alternative in pain relief care.
- Understanding Personalized Thermal Therapy for Pain Relief
- Assessing Individual Needs for Effective Thermal Therapy Plans
- The Role of Temperature Variations in Thermal Therapy Protocols
- Types of Thermal Therapy Techniques and Their Application in Pain Management
- Crafting a Tailored Thermal Therapy Regimen: A Step-by-Step Guide
Understanding Personalized Thermal Therapy for Pain Relief

Individuals seeking relief from chronic or acute pain may find solace in personalized thermal therapy, a modality that leverages controlled heat (hyperthermia) or cold (cryotherapy) applications to manage discomfort. This treatment is tailored to the unique physiological and pathological conditions of each patient, ensuring that the temperature applied is optimal for their specific pain presentation. The application of thermal therapy can improve local blood circulation, reduce inflammation, and stimulate cell repair mechanisms, making it a versatile option for various types of pain, from musculoskeletal disorders to neuropathic conditions.
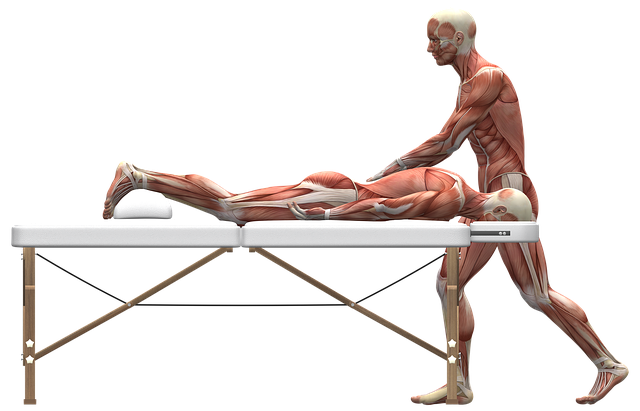
Practitioners who specialize in thermal therapy employ a variety of methods, including thermal agents like ice packs, heating pads, or advanced equipment such as focused ultrasound devices that deliver precise heat deep into the tissues. The personalization aspect is crucial, as the intensity and duration of thermal therapy are carefully adjusted to the patient’s response to treatment. This individualized approach not only enhances the efficacy of pain relief but also minimizes the risk of adverse effects, thereby creating a safe and effective path to recovery. Regular assessments and adjustments ensure that the therapy continues to align with the evolving needs of the patient throughout the course of treatment.
Assessing Individual Needs for Effective Thermal Therapy Plans
Personalized thermal therapy plans are pivotal in achieving effective pain relief due to the unique physiological responses that individuals exhibit. A thorough assessment of each patient’s condition is essential, as it determines the most suitable application of heat or cold. Healthcare providers must consider factors such as the type and intensity of pain, underlying medical conditions, and patient tolerance to temperature variations. By integrating this information, therapists can tailor thermal therapy treatments to optimize healing while minimizing discomfort or potential adverse effects. This individualized approach ensures that the chosen therapeutic temperatures are safe and beneficial for the specific pathology at hand, thereby enhancing the overall efficacy of thermal therapy in pain management.
Furthermore, the selection of temperature modalities, whether it be hot packs, cold compresses, or a combination of both, should be guided by the patient’s feedback and response to initial treatments. Regular monitoring and adjustments to the treatment plan are necessary to ensure that the thermal therapy is delivering the intended pain relief effects without causing harm. This adaptive approach allows for continuous improvement of the therapy plan, ensuring it remains aligned with the patient’s evolving needs and responses. The ultimate goal is to provide a personalized thermal therapy regimen that is both effective and comfortable for the individual, thereby facilitating their journey towards pain alleviation.
The Role of Temperature Variations in Thermal Therapy Protocols

In crafting personalized thermal therapy plans for pain relief, the strategic application of temperature variations plays a pivotal role. The use of alternating hot and cold packs can enhance the efficacy of treatment by promoting blood flow and reducing inflammation. For instance, heat therapy increases circulation to an area, which can help ease stiffness and muscle spasms, while cold therapy helps to constrict blood vessels, reducing swelling and pain. This dual-approach not only addresses the immediate symptoms but also aims to facilitate a healing environment within the affected tissue.
Thermal therapy protocols are tailored based on individual patient responses and specific medical conditions. For example, acute injuries may benefit from the vasodilation effects of heat early on, while chronic pain conditions might require the analgesic properties of cold to manage ongoing discomfort. The precise control of temperature allows for a customized approach that can be adjusted as the healing progresses, ensuring optimal comfort and therapeutic outcomes for the patient.
Types of Thermal Therapy Techniques and Their Application in Pain Management

Thermal therapy encompasses a range of treatments that utilize temperature-controlled modalities to manage pain. Among these, hot packs and cold compresses are the most commonly used at home or in clinical settings. Hot therapy, such as moist heat applications like a whirlpool bath or a heating pad, is particularly effective for musculoskeletal conditions like muscle strains and arthritis. It increases blood flow and relaxes tight muscles by penetrating deeply to soothe sore areas. Conversely, cold therapy, including ice packs or gel wraps, is often used for acute injuries or post-surgery recovery to reduce swelling and inflammation. Both modalities can be applied independently or in a sequence known as “thermotherapy,” where heat and cold are alternated at specific intervals to enhance their therapeutic effects. The choice between hot and cold therapy, or the decision to combine them, depends on the type of injury, the patient’s comfort level, and the stage of healing. In clinical settings, more sophisticated thermal therapies like shortwave diathermy and ultrasound therapy are also employed. These advanced techniques offer deep-heating capabilities without affecting the overlying tissues, making them ideal for treating deeper structures such as ligaments, tendons, and joints. The precision of these methods allows healthcare providers to tailor thermal therapy treatments to the individual needs of patients seeking pain relief.
Crafting a Tailored Thermal Therapy Regimen: A Step-by-Step Guide

When incorporating personalized thermal therapy plans into a pain relief regimen, it is imperative to consider the individual’s specific condition and response to heat or cold. The initial step involves assessing the type of pain and its underlying cause, as different conditions may benefit from varying temperature applications. For instance, muscle strains often respond well to alternating hot and cold therapy, which can improve circulation and reduce inflammation. Once the pain’s nature is understood, select appropriate thermal modalities, such as heated pads for muscular aches or ice packs for acute injuries. Subsequently, tailor the treatment frequency and duration based on the patient’s comfort level and the medical advice provided. It is crucial to monitor the skin’s reaction throughout the therapy to prevent tissue damage; adjustments should be made as needed. Progression to more advanced thermal applications, such as therapeutic ultrasound or shortwave diathermy, may be indicated based on clinical judgment and patient progress. Throughout this process, regular evaluation of pain levels and function is essential to ensure the therapy is effectively meeting the individual’s needs.
Personalized thermal therapy emerges as a versatile and effective modality for pain relief, catering to the unique physiological and psychological needs of individuals. By evaluating individual circumstances and integrating various temperature-based techniques, healthcare practitioners can craft tailored thermal therapy regimens that promote healing and comfort. This comprehensive guide illuminates the critical aspects of designing such protocols, ensuring that patients receive the most beneficial approach for their pain management. Embracing the nuances of thermal therapy, from its mechanisms to its application, underscores a transformative shift in pain relief strategies. As healthcare advances, personalized thermal therapy stands out as a promising and adaptable solution for those seeking effective, non-invasive pain relief options.
